
Home » Thermography stirs debate among Spokane breast cancer screening experts
Thermography stirs debate among Spokane breast cancer screening experts
Advocates, detractors argue its role in breast cancer detection; both laud mammograms
January 5, 2012
A lesser-known form of body imaging called thermography, which has been said in some cases to help doctors detect early-stage cancerous or pre-cancerous lesions in a patient's breasts, has seen fluctuations in usage during the last several years and seems to be gaining in practice again, providers here say.
While thermography has been approved since the early 1980s by the U.S. Food and Drug Administration only as an adjunct to mammography, there still is a large amount of controversy in the medical field surrounding its reliability and effectiveness in detecting breast cancer.
Both advocates and opponents of thermography here say that those conflicting opinions may leave some women confused when making decisions about breast health.
Spokane is host to two providers who offer thermography, also referred to as digital infrared thermal imaging, as an alternative method to aid in the detection of breast cancer or potentially pre-cancerous areas of the breast tissue.
Both providers, Spokane-based Windrose Naturopathic Clinic LLC and Spokane Valley-based Empire Digital Imaging, say they're aware of the scrutiny surrounding thermography. They assert, though, that they make sure their clients know that the screenings shouldn't be considered a replacement for annually recommended mammograms for women age 40 and older.
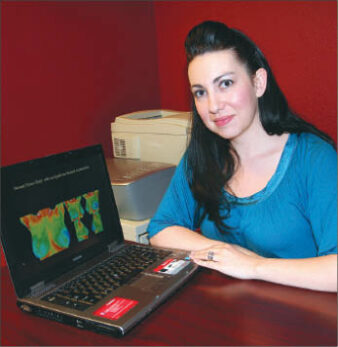
Karla Porter, a certified thermography technician with Windrose Naturopathic Clinic, located at 1137 W. Garland, says thermology is an early risk-assessment tool that uses an infrared camera to measure the body's output of heat at the surface of the skin. While it can be used to aid in the diagnoses of many body ailments, one of thermography's most common applications is in breast imaging, she says.
The concept behind thermography is that the infrared camera is able to detect "hotter" areas of the upper body that then are visible on a color-gradient and digitally-generated thermal image of the body, Porter says. Those warmer areas could show up because of an abnormality in a breast, she says, such as a potentially cancerous area of tissue that's fed from its own blood supply, which thus could be shown by the camera as a "warm" spot when compared with other areas of the body.
"The best way to describe thermography is that it's a monitoring system and it can act as an early-warning system up for several years before you can see a mass on a mammogram," Porter asserts. "You can see the beginning disease process on a thermogram. It looks at the cellular level of the breast and a mammogram looks at the structure or anatomy, so they are two technologies that complement each other."
Aside from generating a thermal-image scan of the body, the camera also records temperature readings of different points on the patient's body, she says.
Digital thermal image scans can be produced both in a grayscale and full-color spectrum. In a color image, white, red, orange, and yellow are considered "warm," while greens, blues, and purples are defined as "cold" areas, she says.
"We are very symmetrical so we should have similar temperature readings on both sides," she says. "The breasts are further away from the body so they're cooler and should be in the blue-green scale, and there is suspicion if they don't look the same on each side or (if they) show the warmer colors."
Porter claims that thermography alone has been studied and shown to be about 90 percent accurate in the detection of cancer or pre-cancerous masses in the breast tissue, and she says that when used in conjunction with mammography, that rate climbs to 98 percent.
Not all medical providers here agree with those statistics, however, including some of the Spokane area's largest providers.
Inland Imaging LLC, the big Spokane-based radiology group, doesn't offer thermography as a modality of breast imaging, and the imaging provider's stance largely is based on that of the FDA, says Dr. Florence Gin, a radiologist with Inland Imaging who specializes in breast-imaging services.
"Screening mammography is the only breast-imaging modality that has been shown to decrease morbidity and mortality," Gin says. "Thermography has not been shown to decrease morbidity and mortality."
Inland Imaging has published on its website an official statement regarding its position questioning the effectiveness of thermography as a means of breast cancer detection.
Gin says that in addition to screening and diagnostic mammography services, Inland Imaging offers a range of other types of breast imaging including breast MRI, breast ultrasounds, and positron emission tomography (PET) scans of the breast.
"We make sure to give a complete package so we can tell her, 'We aren't finding anything,' or, 'This is the next step and you need a biopsy or you need to see a breast surgeon,' and we give them guidance," Gin says.
She adds that Inland Imaging often sees patients who've had what was interpreted as a normal thermogram and yet were found to have breast cancer through the use of other diagnostic imaging tools. The radiology group also often sees women who have had what's considered an abnormal thermogram, but when they were screened through other methods were found not to have any form of cancer or pre-cancer, she says.
"In theory, thermography has a seed of truth, but the problem with the research I've looked at is that the sensitivities and specificities for it are all over the place," Gin says.
Jan Robins, Inland Imaging's mammography manager, says she's noticed that the prevalence of the use of thermography seems to come and go in waves, and that now she's seeing more women come in than in recent years who've had the screening done elsewhere.
"It's back in the news again and I'm not sure why it's come to the forefront, but the women that come to see us, they're frustrated or angry that they had it and didn't have a mammogram and now we're doing mammograms," Robins says.
In Spokane Valley, certified clinical thermographer Justice Naccarato says she performs on average of 35 screenings each month for women who want to have their breasts scanned for abnormalities.
Naccarato and her husband, Brian, own Empire Digital Imaging, located at 618 N. Sullivan, which they've operated in the Inland Northwest since 2008.
Naccarato says her clients discover her services through a number of outlets, including referrals from some area doctors, as well as women who've researched thermography on their own and came across her business.
The actual process for a breast thermogram takes about 15 minutes during which five images are captured showing different angles of the patient's chest area, she says. The images then securely and electronically are sent to a doctor who's been trained on how to read and interpret them, she says. A report on the patient's thermogram later is sent back to either the patient or to her referring doctor for further evaluation.
Naccarato stresses that she only is trained to capture the thermal images and to walk the patients through the process.
"As technicians, there is a fine line that we walk," Naccarato says. "I let them know the FDA approval and our role, and they have to make any decision with their doctor."
Naccarato says she's seen a noticeable increase in the number of women coming to her clinic for a breast thermogram in the last year.
Because thermography still only is considered an adjunct to mammography when used for breast imaging purposes, most insurance pro-viders don't cover the procedure's cost, she says. Patients at Empire pay $150 for their first imaging session, and each additional thermography visit after that is $110, she says.
Naccarato says the American College of Clinical Thermology, based in Fort Myers, Fla., recommends that women who are having a thermogram for the first time come back three months later for a second imaging session. She says that's because one way of identifying abnormalities is by comparing images.
The American College of Clinical Thermology is the organization through which Naccarato received her training and certification in thermography, she says.
"With thermography, you have a thermal image that is like a fingerprint that's unique to you, and it's most beneficial when we screen regularly, so if women come each year, we can help with detection," she asserts.
"The only downfall is that we can catch things in their earliest stages and you can't biopsy it because it's so small, but then it can be monitored with ultrasounds and MRIs and you have a heads up and know you might be at risk," she adds.
The International Academy of Clinical Thermology, based in Redwood City, Calif., is the other main accrediting and standardization group and is the organization that accredited Windrose Naturopathic Clinic, says its thermography technician Porter.
Porter and Naccarato both assert that women should start receiving annual thermograms starting in their early 20s.
Porter adds that when she administers a thermography session to one of her patients, she also performs a clinical physical breast exam.
Like Naccarato, Porter says she makes sure her patients understand that they shouldn't be replacing regular mammograms with thermography. Yet, she says the negativity surrounding thermography and the arguments over its effectiveness are disconcerting to her.
Both the American College of Radiology and the Society of Breast Imaging, two nonprofit industry organizations, have issued recent public statements stating non-support of thermography as a breast screening tool even as an adjunct to mammography.
"All I can say is that any naysayer has not looked into the technology within the last 15 to 20 years," Porter says.
Spokane-based Rockwood Clinic PS doesn't offer thermography as a breast imaging service and declined to comment on the methodology.
Latest News
Related Articles



