
Home » Providence Health prepares for Epic shift in electronic health records
Providence Health prepares for Epic shift in electronic health records
Organization's operations here are scheduled to have system on line by year-end
February 16, 2012
Providence Health & Services, the big health services network that includes Spokane-based Providence Health Care, is poised to do something Epic with its health records system, a move that it expects will make its operations more efficient.
Providence is preparing to install customized health records technology developed by Madison, Wisc.-based Epic Systems Corp. at all of its hospitals, medical clinics, and Providence-owned physician practices in Washington, Oregon, Alaska, Montana, and California. In all, the effort involves upgrading the health records systems at 27 hospitals and more than 400 clinics, including Providence Sacred Heart Medical Center & Children's Hospital, Providence Holy Family Hospital, and a number of other medical facilities and physician practices in the Spokane area.
"Epic creates an integrated and unified patient-centered database," Providence Health Care Chief Executive Mike Wilson says in a prepared statement. "It centralizes information, assisting caregivers in making the best decisions for the patient, and removes unnecessary duplication while also adding safeguards that ensure the highest quality of care."
The system is like an Epic health records system Group Health Cooperative installed at its Spokane operations in 2005 and has been using since then. Similarly, Rockwood Health System, of Spokane, and a group of six Eastern Washington rural hospitals are negotiating with a Seattle-based health care information technology company to install a system that would allow those medical facilities to track patient referrals and more easily share medical records.
Two Providence employees in Spokane, Sherry Maughan and Tami Klein, are in the middle of three-year stints as directors for Epic's deployment in Eastern Washington. Maughan is overseeing the system's implementation at Providence's acute-care hospitals, and Klein is handling deployment at offices outside of the hospitals that are known broadly as ambulatory services.
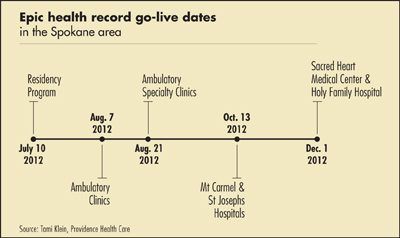
Starting in July, Providence's Eastern Washington physician practices and other ambulatory services will go live on the Epic system. Klein says those offices will continue to come on line with the system through August and into fall.
Two rural hospitals in Eastern Washington—Providence Mount Carmel Hospital, in Colville, and Providence St. Joseph's Hospital, in Chewelah—are scheduled to begin using Epic in October, Klein says, and Sacred Heart Medical Center & Children's Hospital and Providence Holy Family Hospital, are scheduled to go live Dec. 1.
Klein says Providence employs a total of about 7,000 people in Eastern Washington, and those involved in patient care will receive just-in-time training on the new system in the days before it goes live at the facilities in which they work.
Both Maughan and Klein describe the system as a major upgrade compared with the medical records systems in place presently.
Providence's acute and ambulatory operations currently have separate health records systems that aren't connected. Consequently, a patient who is referred to a hospital from a physician's practice typically is asked the same questions repeatedly because hospital staff doesn't have access to records from the doctor's office.
Once Epic is in place, Providence hospital staff will have access to records from the physician's practice, allowing them get up to speed on a patient's condition more quickly.
"It's a well thought-out tool," Maughan says. "There will be a lot less redundancy."
With access to a physician's records, hospital staff doesn't have to rely on a patient as heavily to relay the specifics of the medical condition.
For a referring physician, the system incorporates scheduling referrals that can be tracked, ensuring that a patient has received the necessary follow-up care.
Klein says, "From a patient's perspective, this is huge," adding that Providence's mantra for its patients while setting up the Epic system is, "Know me. Care for me. Ease my way."
She says patient themselves will be able to access their own medical records through Epic.
"That's a huge win for patients in the community," she says. "The patient is involved as part of the care team. The way our system is built, it engages the patient in the care in a way we haven't in the past."
Dr. Tom Schaaf, assistant medical director of the Eastern Washington/North Idaho for Group Health Cooperative, says the Epic feature that allows patients to retrieve their own health records has proven to be a popular feature. While some physicians at first had reservations about sharing information and about patients' ability to interpret that data, most have become more comfortable sharing that information and answering questions from patients via email, Schaaf says.
Group Health implemented its Epic system in Spokane in 2005, Schaaf says. At that time, he says, its medical staff was making the jump from paper charts to electronic records, and that transition carried a steep learning curve for its physicians and other caregivers.
"It's like the difference between a book and a Kindle," Schaaf says. "With a book, you know physically where to find something. With a Kindle, you have to figure out where to look. It's a whole different thought process when you're going in to see a patient."
Schaaf points out, however, that Providence physicians already use electronic records systems, so the learning curve shouldn't be as steep as it was for Group Health in the mid-2000s.
With Epic, it should be easier for Group Health physicians to receive lab results and notes from patient visits to Providence hospitals and doctors' offices, he says. Also, physicians should be able to communicate more efficiently with those at Providence, says Schaaf, a family physician who also has worked as a hospitalist. Ultimately, he says, that could lead to fewer unnecessary physician visits and faster treatment for patients.
For example, if Schaaf currently is treating a patient who appears to be having heart problems, he would refer that patient to a cardiologist. The patient then would make an appointment that in all likelihood would be four to six weeks later. With both Group Health and Providence on Epic, Schaaf says it could be easier to link up with a cardiologist, present the patient's symptoms, then receive instruction for tests or other treatment options.
"It decreases unnecessary visits and gets the right care done more quickly," Schaaf says.
In the Rockwood Health System, which includes Deaconess Hospital, Valley Hospital, and Rockwood Clinic, a system developed by Seattle-based Clarity Health Services Inc. could be installed later this year if contracts between Rockwood and Clarity are approved.
David Kimberling, Rockwood Health executive director for strategic business development, says the organizations are in the final stages of contract negotiations now.
Such a system would enable Rockwood to receive referrals electronically from some rural Eastern Washington hospitals. Those rural medical centers are Lincoln Hospital, in Davenport; Newport Hospital & Health Services, in Newport; Coulee Community Hospital, in Grand Coulee; Garfield County Hospital, in Pomerory; Odessa Memorial Healthcare Center, in Odessa; and Whitman Community Hospital, in Pullman.
Latest News
Related Articles




