
Home » As obesity, diabetes rise, perinatal services grow here
As obesity, diabetes rise, perinatal services grow here
June 6, 2013
Due partly to the rising prevalence of obesity and diabetes, the Spokane area is seeing growth in perinatal, or maternal-fetal medicine, services, which strive to ensure the best possible outcomes in high-risk pregnancies.
A maternal-fetal medicine program at Deaconess Hospital that launched fully about a year ago and one at Providence Sacred Heart Medical Center & Children's Hospital that was established about seven years ago both expect to grow in response to steadily escalating demand, program leaders say.
"The program is growing so fast that we had to hire not three but four sonographers, a nurse practitioner, a genetic counselor, and we're working to bring on more maternal-fetal medicine doctors as needed," says Dr. Reinaldo Acosta, perinatologist and program director for Deaconess Maternal-Fetal Medicine, with Obstetrix of Spokane.
Dr. Douglas R. Barber, perinatologist at Sacred Heart's Center for Maternal-Fetal Medicine, says, "America's not getting skinnier, for sure. That certainly trickles down to pregnancy. We're only gaining more and more (patients) over time."
Maternal-fetal medicine is the branch of obstetrics that focuses on the medical and surgical management of high-risk pregnancies. Specially trained obstetricians who practice maternal-fetal medicine also are known as perinatologists.
Some of the services provided by maternal-fetal medicine centers include diabetes care, detailed ultrasound imaging of the fetus, and a screening test called chorionic villus sampling that can identify genetic problems with the baby. Other services include genetic amniocentesis, which is another test that can identify genetic disorders such as Down syndrome and spina bifida, and the management of twin or triplet pregnancies.
Despite the rising number of patients coming to the Spokane programs, Acosta and Barber both say they believe the perinatal services now being provided here are having a positive impact, such as through fewer premature births.
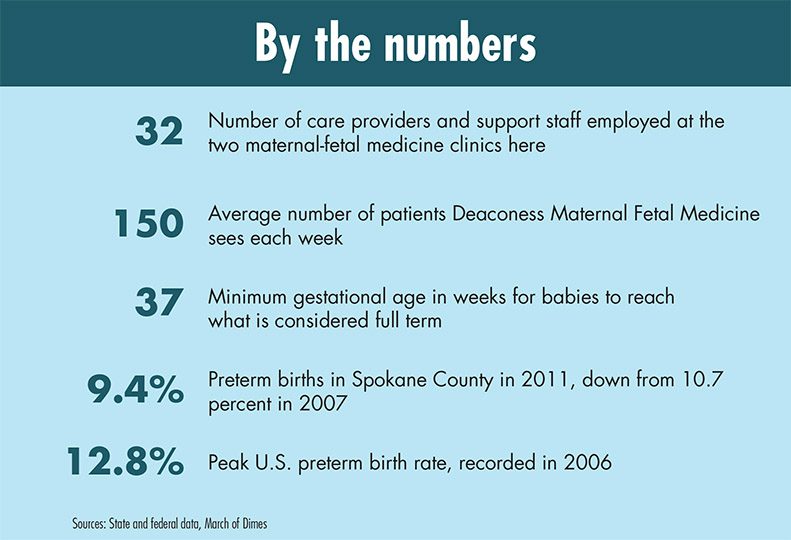
Statistics weren't readily available from the two hospitals to substantiate that perceived decline. However, data compiled by the Spokane Regional Health District show that preterm births—defined as those with a calculated gestational age of less than 37 weeks—fell significantly in Spokane County from 2007 to 2012, even as the number of new mothers here who were obese before pregnancy and had diabetes during pregnancy climbed substantially.
That trend mirrors what's been happening nationally.
The March of Dimes reported in its 2012 Premature Birth Report Card released last November that the rate of premature births dropped nationally for the fifth consecutive year in 2011 to 11.7 percent, the lowest rate in a decade.
Oregon and three northeastern U.S. states earned an "A" in the Report Card as their preterm birth rates met the March of Dimes' 9.6 percent goal. Oregon was at a 9.1 percent premature birth rate, while Washington, Idaho, and Montana were at 9.8 percent, 10.2 percent, and 10.8 percent, respectively, which earned them a "B" in the rankings. Although the U.S. preterm birth rate improved, it again earned a "C" in the March of Dimes grading.
The U.S. preterm birth rate peaked in 2006 at 12.8 percent after rising steadily for more than two decades, according to the National Center for Health Statistics. The five-year decline since then has given thousands of additional babies a healthy start in life and has saved billions of dollars in health and social costs, March of Dimes says.
March of Dimes' President Dr. Jennifer L. Howse attributed the five-year decline in premature births to an expansion of successful programs and interventions across the country, including actions taken by state officials.
Reducing premature births is one important goal of the perinatal programs here, but the programs are focused more broadly on using skilled specialists and a coordinated approach to deal with all of the needs and crises that might arise in high-risk pregnancies, leaders of the programs say.
Acosta says a pregnancy can be high risk for several main reasons. The patient might have complications, such as a heart condition, hypertension, or diabetes, or might experience preeclampsia, pre-term labor, or a rupture of the membrane, or might be expecting multiple babies, he says. Or, the patient might be doing well, but the fetus might have some malformations or disorders, he says.
Being able to respond quickly and effectively to complications related to each of those conditions requires assembling a talented team of care providers, he and Barber say.
At Deaconess, Acosta says, "I was able to customize the team with the key players I really want to have a successful perinatal center." He adds, "I'm really happy with how it's going."
Barber says, "I'm very pleased because I don't think when I came here I knew the breadth of subspecialty care available in the community. I have such breadth of support I'm really excited for the future here."
A small handful of perinatologists here are among what is said to be only about 1,800 perinatologists nationwide. In addition to four years of residency training in obstetrics and gynecology, the maternal-fetal medicine subspecialist has received two to three years of education in the diagnosis and treatment of disorders of the mother and fetus.
Acosta, a native of Colombia, comes from a family of obstetricians.
"At a very young age, I was hearing about these conditions," he says, " and hearing about how rewarding it is to take a challenging patient with a guarded prognosis and in the end turn out to have a normal, healthy baby."
He earned his medical degree from Javeriana University in Bogota, served his obstetrics and gynecology residency at the University of Puerto Rico in San Juan, and received fellowship training in maternal-fetal medicine at Harbor-UCLA Medical Center and Stanford University Medical Center in California.
He then returned to Colombia and developed a maternal-fetal medicine center at the nonprofit Fundacion Cardioinfantil, in Bogota, where he worked for almost three years.
Acosta says he then was hired by Providence Physician Services to develop a maternal-fetal medicine center here at Sacred Heart Medical Center, starting that unit "from scratch" in late 2005, and remained at the hospital until early 2010.
He moved to the Midwest, and joined the faculty at the Southern Illinois University School of Medicine as an assistant OB-GYN professor, specializing in maternal-fetal medicine, before being recruited to come back to Spokane.
Deaconess Hospital hired Obstetrix Medical Group, a Florida-based practice that claims to be the nation's leading provider of maternal-fetal, newborn, and pediatric subspecialty physician services, to attract a program director to Deaconess "to develop exactly the same thing we did at Sacred Heart," Acosta says. That recruitment effort convinced him to return, he says, adding that the Obstetrix unit that he is part of operates under that medical group's Seattle division.
"I think this was a good opportunity for me to join them. I love living in Spokane," he says.
The Deaconess maternal-fetal medicine program is located on the hospital's second floor and includes a total staff of 16 people, counting care providers and people in support positions. Along with working with patients there, Acosta leads an outreach program through which he travels to rural communities throughout the Inland Northwest to help educate care providers about perinatal-related topics and also conducts a monthly videoconference on related topics of interest to them.
Barber is one of two perinatologists currently on staff at Sacred Heart's Center for Maternal-Fetal Medicine, along with Dr. Jorge E. Tolosa, and a third perinatologist, Dr. Gabor Mezei, will be joining them in July. Barber is a Great Falls, Mont., native who earned his medical degree from the University of Washington, served his residency at the University of California, Davis Medical Center, and also received his fellowship training there.
"One of my largest goals, just being from this area, was really bringing very directed subspecialty care back to some smaller communities," Barber says.
He joined Sacred Heart in September 2011, and says, "I was happy to find an opening here at Sacred Heart at the time. What they had already built was more than I was hoping for." That included a "giant team of pediatric subspecialists," he says, adding, "It's been really rewarding to be part of that."
The Sacred Heart center is located on the main floor of the hospital, in the women's health center in the west wing, and, like the Deaconess program, includes a total staff of 16 people.
Up Close
Related Articles




