
Home » Valley physician treats joint pain with sugar solution
Valley physician treats joint pain with sugar solution
Prolotherapy said to help create connecting tissue
December 3, 2015
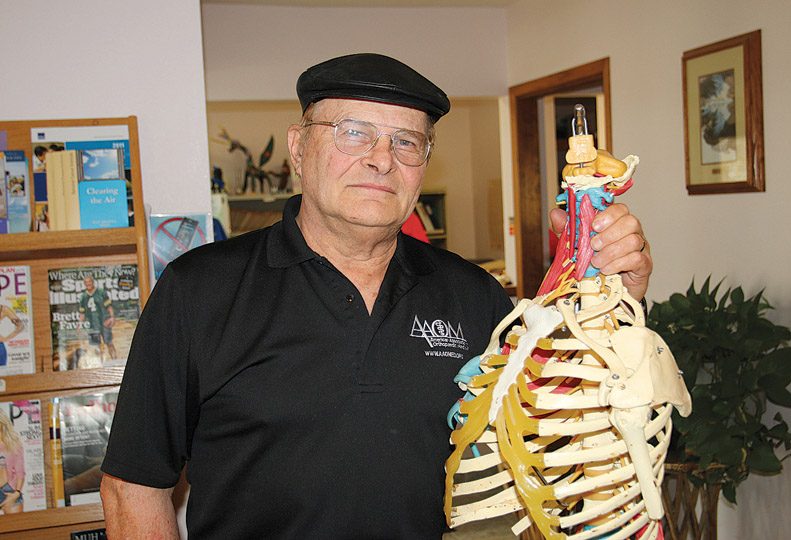
A Spokane Valley physician specializes in an alternative therapy that he says helps relieve some common forms of joint and muscle pain.
Dr. Merle Janes, owner of Valley Rehabilitation, says the treatment, called prolotherapy, involves injecting a solution consisting largely of sugar water into tendon and ligaments where they connect with bones to treat musculoskeletal pain caused by injury and aging.
Prolotherapy assists the body’s natural ability to repair and strengthen loose ligaments and tendons and the joints they hold together, he contends.
“It’s elegant, simple, inexpensive, safe, and has good results,” he asserts.
Though the theory of how it works has evolved with practice and research, it’s currently thought that the sugar solution acts as a mild irritant that causes the body to regenerate ligament and tendon fibers that connect muscle and bone, Janes says.
The new tissue repairs connections between injured or stressed tendons, ligaments, and bones and tightens loose joints, he claims.
“People with pain in their muscles, tendons, or ligaments probably can benefit from prolotherapy,” Janes says. “It stimulates the body to heal better.”
Prolotherapy isn’t used to treat internal pain or cancer-related pain, he says.
When a body is injured, it’s supposed to build new tissue, but that doesn’t happen sometimes, he says, adding that some musculoskeletal injuries stop healing because certain proteins, called growth factors, aren’t present.
Prolotherapy helps trigger growth-factor production, he asserts.
Treatment sessions for a knee joint cost $150 each, Janes says.
“It’s rare to have a single treatment do everything,” he says.
Most treatments involve five or six sessions, Janes says, adding that few prolotherapy treatments require more than seven or eight sessions to yield results.
Most patients opt for four weeks between sessions, he says.
Treatments might look more painful that they really are, Janes says.
“The area to be treated is cleaned and numbed, and the objective is to use the thinnest needle possible,” he says. “The first treatment is the worst, because people don’t know what to expect. The worst that happens is a small amount of bruising.”
Janes says he treats five to seven patients a day with prolotherapy at his office at 1414 N. Vercler, east of the Valley Hospital complex, where he works with one assistant.
“The most complicated treatment would be one with several injury sites,” he says. “If it’s just knee pain, it’s simpler.”
Janes has been practicing prolotherapy here since 1996.
He says that some patients come to him because they’ve heard of and are interested in prolotherapy.
Most often, though, new patients are referred to him by their friends or family members who’ve had good results.
Since 2001, Janes has treated patients in the Seattle area four days a month.
“I knew people over there, and I asked around, and prolotherapy wasn’t being done by anyone,” he says. “Since that time, others are doing prolotherapy.”
Janes says he’s not aware of other prolotherapy practitioners in the Spokane area.
Prolotherapy has some ancient roots going back to Greek physician Hippocrates, and the principle also was used in early Egyptian medicine, he says. Starting in 1939, U.S. physician George Hackett developed the injection-based therapy practiced today.
Janes says he learned prolotherapy techniques from Drs. Gustav Hemwall and Jeff Patterson, two other pioneers in modern prolotherapy.
He says he’s not just a prolotherapy practitioner, but he’s also a patient. He says he’s had prolotherapy treatments on his neck, lower back, and knees.
The most widely used prolotherapy solution consists of a mixture of the simple sugar dextrose, water, and a small dose of Lidocaine as a temporary numbing agent.
Another type of prolotherapy uses injections of platelet rich plasma, which is derived from the patient, Janes says.
PRP prolotherapy has gained some fans among professional athletes who say it can help repair certain musculoskeletal injuries quickly and without surgery, he says.
“The basic idea is the same in that it causes new tissue to grow,” says Janes, who also offers PRP prolotherapy.
PRP is more costly than dextrose prolotherapy because collection kits, which concentrate platelets from the patient’s own blood, are expensive.
Janes teaches prolotherapy techniques to other physicians through the Madison, Wis.-based Hackett-Hemwall Foundation, which trains physicians every March at a medical missionary in Honduras and holds a prolotherapy conference every October in Wisconsin.
He claims the number of physicians practicing prolotherapy in the U.S. is in the thousands and growing.
Not everyone is convinced about prolotherapy, though, and many health insurance carriers deny coverage for it.
Aenta, the big Hartford, Conn.-based health care benefits provider, for example, considers prolotherapy experimental and investigational, citing “inadequate evidence of its effectiveness,” the company’s website says. Aetna is scheduled to review its policy regarding prolotherapy in February.
On the other hand, the American Association of Orthopaedic Medicine, which promotes education for nonsurgical treatment of musculoskeletal problems, recognizes and teaches prolotherapy, and encourages health insurance carriers to provide coverage for it.
The U.S. National Library of Medicine lists on its PubMed.gov website a number of recent articles and reviews regarding pilot-level studies that suggest positive outcomes with prolotherapy for certain musculoskeletal disorders, although nearly all of the literature recommends that larger clinical trials be conducted.
Latest News Special Report Health Care
Related Articles




