
Home » Women's surgery center opens
Women's surgery center opens
Practice at Sacred Heart uses robotic operating equipment, seeks to reduce trauma
March 26, 2009
In anticipation of a growing demand for less traumatic surgery for women, Providence Sacred Heart Medical Center & Children's Hospital has launched a practice called the Center of Gynecology Robotics & Minimally Invasive Surgery.
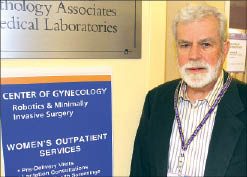
The practice, which opened March 16, is headed by obstetrician-gynecologist Dr. R. Steven Brisbois, who has a longtime relationship with the hospital. The new center occupies 2,500 square feet of floor space on the first floor of the Women's Health Center in the hospital's west tower. Brisbois is the lone physician in the practice, which has a staff of five employees, including two nurses.
Brisbois also was hired as medical director of the Women's Health Center in January.
"I'm becoming an employee of Sacred Heart after 29 years of private practice," he says.
Brisbois co-founded Northwest Ob-Gyn, here, in 1980 and left there to concentrate on minimally invasive gynecological surgery at the Center for Reproductive Health, also of Spokane, in 2007.
The new surgical practice will place more emphasis on robotic procedures, he says.
"It's not an effort to compete with local obstetricians and gynecologists," Brisbois says. "I take a lot of complex, difficult cases, including people who are at very high risk for surgery."
He says he began performing gynecological robotic surgery procedures in June 2006, and since then has used robotic equipment in about 200 cases.
In the area of gynecology, robotic surgery is used to perform hysterectomies, to remove uterine fibroids, and to repair some disorders of the pelvic-floor muscles. Uterine fibroids are noncancerous growths of the uterus that sometimes cause pain, bleeding, and fertility problems.
Brisbois describes surgery as controlled trauma. "There is less trauma using robotic surgery," he says.
Gynecological robotic surgery typically involves four or five lower abdominal incisions, each less than an inch. A lens for a binocular camera is inserted into one incision, and thin instruments attached to up to four robotic arms are inserted into the other incisions.
The surgeon controls the robotic arms through a console that provides 3-D views via the binocular camera. The control system translates the surgeon's hand movements to the motion of the surgical instruments.
"It's a blend of scope surgery with microsurgery," Brisbois says.
Most patients who undergo gynecological robotic surgery can go home from the hospital the same day, and return to work within a week.
"The outcome is better for the patient," he says.
The majority of hysterectomies still are done conventionally through an open incision several inches long, requiring longer recovery time. In such cases, "It can be five to six weeks before a patient returns to work," Brisbois says.
Most patients can be candidates for other minimally invasive techniques, which include surgical access through the vagina or straight laparoscopic surgery via small abdominal incisions.
"Patients who are not candidates for those techniques no longer have to have their belly opened in all cases," he says.
Robotic instruments have wrist-like joints and operate at angles in places that otherwise would be hard to access except through a large incision, Brisbois says.
"Robotic surgery allows me to do procedures I couldn't do previously using other minimally invasive techniques," he says. "Candidates for gynecological robotic surgery are women facing the reality that they have to do something and who would be facing a major abdominal incision without the robot."
Such candidates include heavy women, women with large uteruses, and women with multiple fibroids in areas that are difficult to reach.
The number of robotic procedures performed is small compared with conventional and noninvasive procedures, but it's growing, Brisbois says.
Sacred Heart has two da Vinci surgical robot systems, which cost about $1.6 million each. They were made by Intuitive Surgical Inc., of Sunnyvale, Calif. Kootenai Medical Center, in Coeur d'Alene, also has a da Vinci system.
"It takes a lot of capital to start a robotic surgery program," Brisbois says.
He serves as a proctor in gynecological robotic surgery, meaning he's certified to teach, help, and assess whether a physician is developing the proper skills using the da Vinci system.
He's worked with three gynecologists at Sacred Heart who have completed training with the system and now have credentials. Another is in the process of getting credentials.
Brisbois also has acted as a proctor at hospitals in Coeur d'Alene, Missoula, and Tacoma.
The robots also are used by heart surgeons, urologists, and pediatric surgeons. "There's increasing pressure for robot time," he says.
When surgeons first learn robotic surgical techniques, they take more surgery time than with conventional surgery, he says. As they develop their skills, surgeons can become able to perform robotic procedures in about the same amount of time as they can perform conventional surgery, he says.
Surgeries using the da Vinci system generally are covered by insurance plans, including Medicare, that provide coverage for minimally invasive surgery, Intuitive Surgical's Web site says. While it typically is more expensive than conventional surgery, faster patient recovery following a robotic procedure could result in reduced hospitalization costs, the Web site says.
"The big savings that's never calculated by insurance companies is it gets a patient back to her lifestyle and workplace six times faster," Brisbois says. "It benefits society if patients are able to return to their jobs and normal functions at home."
Latest News
Related Articles




